Cervical Disc Arthroplasty (Disc Replacement)
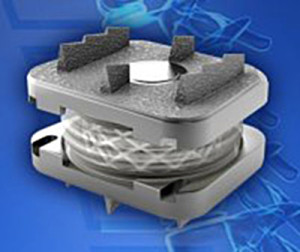
This procedure is a relatively new option to treat cervical disc disease. At present time, only a single level implant is covered by private health funds in Australia. Although there are a number of different implants available on the market, I generally prefer the M6 cervical (see picture).
Indication for a discarthroplasty is a so-called “soft” disc protrusion with a radicular pain pattern (along the arm / hand/ fingers)
 . It also suits best younger patients without advanced degenerative changes in their cervical spine.
. It also suits best younger patients without advanced degenerative changes in their cervical spine.
Standard workup includes cervical X-ray in two planes + dynamic (flexion/ extension/ lateral bending) views, MRI or/and CT.
The procedure is done under general anaesthetic via a small anterior neck incision. Blood loss is minimal as most soft tissue can be mobilised bluntly. As the cervical spine is reached, the correct disc level is identified using X-ray. The appropriate cervical disc is removed using an operating microscope. This allows a proper decompression of the spinal cord and nerve roots. The empty disc space is measured to select the correct sized implant. The artificial disc is placed between the two adjacent vertebra, with the position confirmed with an X-ray. Usually a wound drain is placed into the deep layers of the neck before closure with disolvable sutures.
Postoperatively expect to wear a soft collar for 1 week. Mobilisation is posssible within 12-24 hours. Wound drain removal on day 1 post surgery. Hospital stay is 2-4 days.
Advantages over cervical fusion: preservation of neck movement in the operated level, protection of adjacent levels against rapid degeneration. It can be used in smokers as no bony fusion is required. Ultra-early mobilisation and short recovery allow early return to work and daily activities.